Dementia
Dementia is the progressive impairment of multiple higher cortical functions, such as memory, thinking, orientation, comprehension and language, which impairs activities of daily living. It affects 7-10% of those aged 65+ years, with the rate doubling every 5 years between 60-90 years. There are many types of it, including:
Alzheimer’s disease (50-60%)
Vascular (15-20%)
Dementia with Lewy bodies (10-15%)
Frontotemporal dementia (4-6%)
The general features of Dementia are:
Memory loss
Cognitive impairment
Decline in social behaviour
Symptoms present for 6+ months
Awareness of environment is preserved (not delirium)
Alzheimer’s Disease (50-60%)
This is due to:
Build up of amyloid protein plaques around brain cells and tau protein tangles within brain cells
Cholinergic neuronal cell death
It presents with:
Memory loss
Aphasia - word-finding problems, muddled and disjointed speech
Agitation
Wandering
Personality change
CT Head will show Hippocampal Atrophy (Temporal lobe).
Management:
Acetylcholinesterase Inhibitors (1st line) - Donepezil, Rivastigmine
NMDA receptor antagonist (2nd line) - Memantine
Vascular Dementia (15-20%)
It presents with a sudden onset cognitive decline and stepwise deterioration in those with CVS disease or CVE, as a result of the developing infarcts. The 2 types of it are:
Large vessel - Single infarct, Multiple cortical grey matter infarcts
Small vessel - Multiple lacunar white matter infarcts, Occlusion of single deep penetrating artery
Investigations include:
Detailed hx and examination
Cognition screen
Medication review
Rule out reversible organic causes
MRI
Parkinson’s Disease Dementia/PDD and Lewy Body Dementia/LBD (10-15%)
PDD is diagnosed when there are Parkinsonian symptoms that develop 12+ months before cognitive decline.
60-75% of PD patients develop Dementia
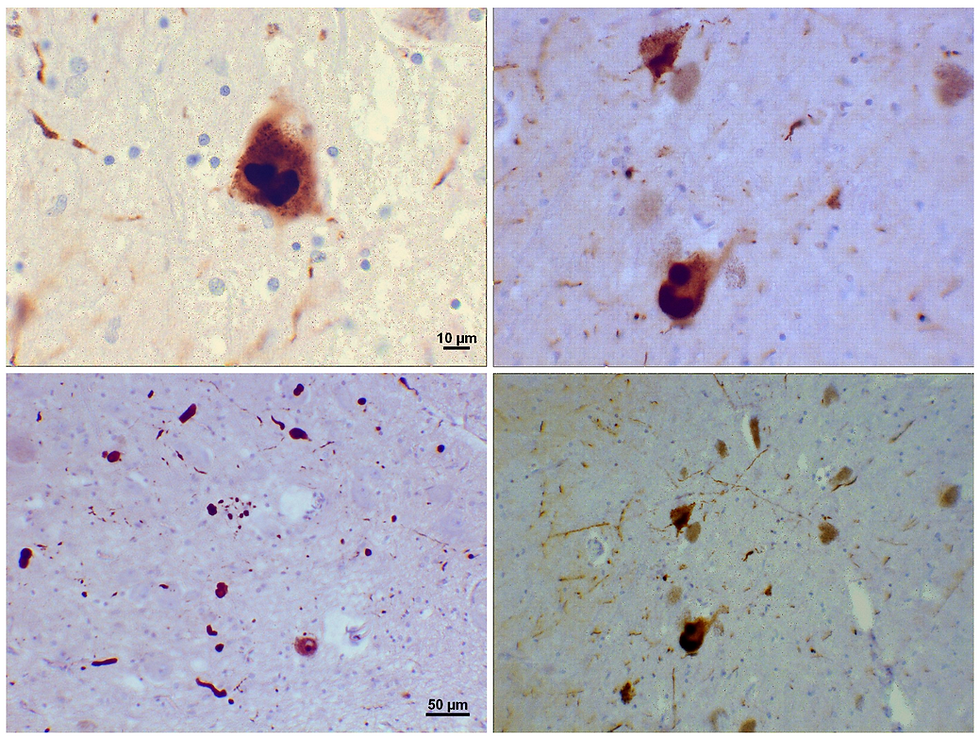
LBD is diagnosed when there are Parkinsonian symptoms that develop 12+ months after cognitive decline. This is due to the formation of Lewy Bodies (alpha-synuclein cytoplasmic inclusions) leading to cognitive decline associated with parkinsonism (bradykinesia, rigidity, tremor).
It presents with 3 core features:
Fluctuating cognition
Parkinsonism
Visual hallucinations
Management:
Acetylcholinesterase Inhibitors (1st line) - Donepezil, Rivastigmine
NMDA receptor antagonist (2nd line) - Memantine
N.B. Avoid Antipsychotics as they work to reduce dopamine, which is already low in those with PD.
Frontotemporal Dementia (4-6%)
It typically occurs at a younger age than other types of dementia, presenting with:
Early personality change and frequently become disinhibited
Poor verbal fluency
One of its causes is Pick’s Disease, which involves the formation of Pick bodies (Tau inclusions) and Pick cells (Ballooned cells).
Imaging shows atrophy of Frontal and Anterior Temporal lobes.

Alcoholism
Wernicke’s Encephalopathy occurs due to a Thiamine (vit B1) deficiency, and presents with Ataxia, ophthalmoplegia, nystagmus, and an acute confusional state. The mammillary bodies (involved in memory function, specifically in its formation and retrieval) in the brain tend to be affected.
Korsakov’s Syndrome is a complication of untreated Thiamine deficiency, and presents with:
Antegrade and Retrograde amnesia
Confabulation (creation of false memories w/o the intent to deceive)

