Malaria
Malaria most commonly occurs in Sub-Saharan Africa. Causes of it are:
P. falciparum (75% of cases) - Most severe form w/irregular fever spikes
P. vivax - Has a period of dormancy in the liver
P. ovale - Has a period of dormancy in the liver
P. malariae
P. knowlesi
Pathophysiology
1st phase is called the Liver phase. This is where sporozoites from the mosquito travel to the liver, enter hepatocytes, and multiply. They then differentiate into merozoites and leak into the blood.
p.vivax and ovale instead become hypnozoites and stay dormant in the liver
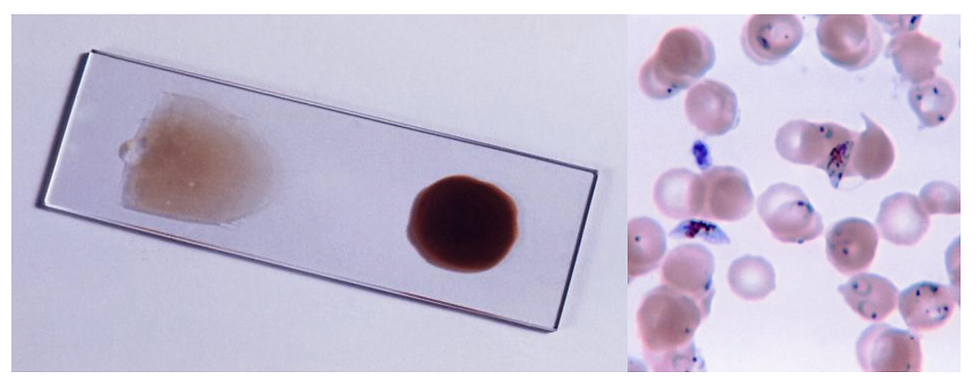
2nd phase is called the RBC phase. This is where merozoites infect RBCs and multiply again before rupturing the cell to infect another. When in the RBC, they also mature into larger Trophozoites (ring in RBC) and Schizonts (brown smudges in RBC as the organism digests haemoglobin to create hemozoin).
The fever spikes are episodic as there’s a period of multiplication and maturation before the RBC ruptures, releasing the merozoites all at once.
Before reinfection of another host body, the merozoites become gametocytes, which stay in the RBCs to be taken up when a mosquito next feeds.
Presentation
The main presenting symptom is Paroxysm, which is a sudden feeling of cold followed by a fever.
P. falciparum - Irregular (called malignant fever)
P. vivax and ovale - Tertian (fever every 48hrs/2 days)
P. malariae - Quartan (fever every 72hrs/3 days)
As the RBCs burst, the patient will present with Haemolytic anaemia - Fatigue, Headaches, Jaundice, Hepatosplenomegaly.
P. falciparium is the most severe type because it covers RBCs with a sticky protein, therefore making them clump together and block vessels. This leads to:
Cerebral malaria - Presents with altered mental status, seizures, coma
Bilious Malaria - Presents with diarrhoea, vomiting, jaundice, liver failure
Ischaemia in lungs, kidney, spleen
Investigations
Thick and Thin blood films - If -ve, it needs to be repeated 2 more times in the next 48 hrs - This is because the parasite may not be released from the RBCs during the time the initial film was carried out.
N.B. In pregnancy, thick films can be -ve even if parasites are present, so a -ve result doesn’t rule out malaria.
Management
Uncomplicated - PO Artemether + Lumefantrine, Proguanil + Atovaquone/Quinine Sulphate/Doxycycline
Severe/complicated - IV Artesunate or Quinine
N.B. Since P. falciparum is the most common and severe type, remember Artesunate and Quinine as the treatment options.
Prophylaxis
General advice - Avoid high-risk areas, DEET spray, Mosquito nets and barriers during sleep
N.B. Sunscreen should be put on before DEET spray.
Before travelling to an area with a high malaria prevalence, patients may be given Antimalarials e.g. Chloroquine, Proguanil, Mefloquine, Doxycycline, Atovaquone.
Important Links:
https://www.nhs.uk/conditions/malaria/
https://bestpractice.bmj.com/topics/en-gb/161
