Leukaemia
Leukaemia is the cancer of a specific bone marrow stem cell line, leading to underproduction of certain blood cells. It's classified into Acute or Chronic, and Myeloid or Lymphoid. Acute differs from chronic as:
Acute is due to impaired cell differentiation, which results in a large number of malignant precursor cells in the bone marrow
Chronic is due to excessive proliferation of mature malignant cells, but cell differentiation is unaffected
N.B. Acute = Immature WBCs proliferating. Chronic = Mature WBCs proliferating.
Leukaemia leads to the suppression of the other cell lines, leading to Pancytopenia.
Types - ALL CeLLmates have CoMmon AMbititons:
< 5 or > 45 - Acute Lymphoblastic leukaemia (ALL)
> 55 - Chronic Lymphocytic leukaemia (CeLLmates)
> 65 - Chronic Myeloid leukaemia (CoMmon)
> 75 - Acute Myeloid leukaemia (AMbitions)
Acute Lymphoblastic leukaemia (ALL)
This is where there's an abnormal proliferation of lymphoid progenitor cells, which infiltrate the normal haematopoietic stem cells of the bone marrow as well as other organs. It typically occurs in children < 5 years. It's associated with Down’s syndrome.
Presents with that of:
Bone marrow failure - pancytopenic symptoms
Organ infiltration - bone pain, painless lymphadenopathy, hepatosplenomegaly, ranial nerve palsies (CNS infiltration), painless unilateral testicular enlargement (testicular infiltration)
Blood film shows Blast cells.

Chronic Lymphocytic leukaemia (CLL)
This is where there's proliferation of functionally incompetent malignant B cells.
Presents typically asymptomatically, but may present with non-tender lympahenopathy, infections, anaemia, bleeding, weight loss.
Blood films shows Smear/Smudge cells - during preparation of the blood film, the aged/fragile cells rupture, leaving a smudge.
CLL can transform into a High-grade lymphoma, and this process is called Richter’s transformation.
Acute Myeloid leukaemia (AML)
This is associated with the myelodysplastic syndromes.
Presents with that of:
Bone marrow failure - pancytopenic symptoms
Organ infiltration - hepatomegaly, splenomegaly, gum hypertrophy
Blood film shows Auer rods.
Chronic Myeloid leukaemia (CML)
This occurs in 3 phases:
Chronic - Often asymptomatic with raised WCC
Accelerated - Abnormal blast cells make up a lot of the bone marrow and blood cells - More symptomatic as pt develops symptoms of bone marrow failure (pancytopenia)
Blast - Abnormal blast cells make up even more of the bone marrow and blood cells - Severe symptoms and pancytopenia, which is often fatal
Presents with:
Massive splenomegaly (>75%)
Weight loss, fatigue, fever, sweating
Bloods - Leucocytosis, in particular raised myeloid cells, including neutrophils, monocytes, basophils, and eosinophils
Usually associated with a Philadelphia chromosome = BCR-ABL t(9;22) gene translocation
It's usually treated with Imatinib (tyrosine kinase inhibitor), with > 80% of pts responding completely to therapy.
N.B. ALL is also associated with the Philadelphia chromosome, where it is a poor prognostic marker.
Complications
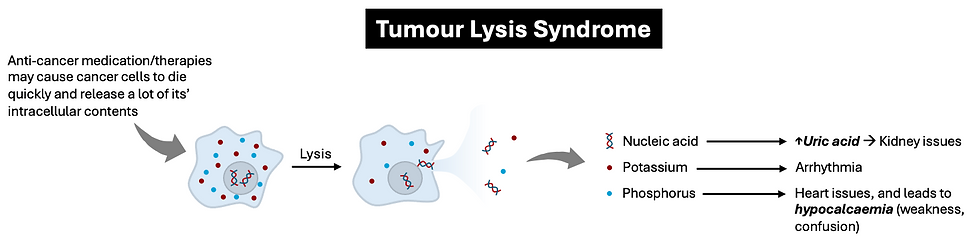
The main complication associated with treating these patients is Tumour Lysis Syndrome, which is the release of uric acid, potassium and phosphate from the cells being destroyed by chemotherapy. It also causes hypocalcaemia due to the raised phosphate.
N.B. The hallmark of this condition is the Raised Uric acid!
Occurs 2 days after receiving high-dose chemotherapy, presenting with dysuria/oliguria, abdominal pain, or weakness.
Easy way of remembering the electrolyte abnormalities is with "raised UPP (uric, potassium, phosphate), and low calcium".
Important Links:
https://bloodcancer.org.uk/understanding-blood-cancer/leukaemia/
https://www.cancerresearchuk.org/about-cancer/leukaemia
https://cks.nice.org.uk/topics/haematological-cancers-recognition-referral/
https://bestpractice.bmj.com/topics/en-gb/273
https://bestpractice.bmj.com/topics/en-gb/274
https://bestpractice.bmj.com/topics/en-gb/275