Obstetric Emergencies
Post-Partum Haemorrhage
This is diagnosed if there's:
500ml loss after vaginal delivery
1000ml loss after c-section
Risk factors - Previous PPH, Multiple pregnancy, Macrosomia, Prolonged 3rd stage, Induced/Augmented/Instrumental delivery, Polyhydramnios
Causes - 4 T's:
Tone - Uterine atony – Most common cause
Contraction of uterus after delivery helps compress the vessels and slows down blood loss
Trauma e.g. perineal tear
Tissue - Retained placenta
Thrombin - Coagulopathy
Prevention:
Emptying bladder before delivery – full bladder can reduce uterine contraction
Active management of 3rd stage with IM Syntometrine
Management:
Mechanical:
Rubbing uterus through abdomen stimulates a contraction
Catheterisation – A distended bladder prevents uterine contractions
Medical:
Oxytocin
Ergometrine – Stimulates smooth muscle contraction
Contraindicated in gestational hypertension as it raises BP
Carboprost or Misoprostol – Prostaglandin analogue
Caution in asthmatics
Tranexamic acid – Antifibrinolytic for high-risk patients
Surgical:
Intrauterine balloon tamponade – Inflatable balloon into uterus to press against the bleeding
B-Lynch suture around uterus to compress it
Uterine artery ligation to reduce blood flow
Hysterectomy – LAST RESORT - Will stop bleeding and may save the mother’s life
Secondary PPH - This is where there's excessive bleeding 24 hours – 12 weeks post-partum. It's most commonly caused by Retained Products of Contraception (RPOC) or Endometritis (infection). These patients should be investigated with a:
TVUS done to check for retained products
Endocervical/high vaginal swabs for infection
Maternal Sepsis
This is most commonly caused by Chorioamnionitis, which is an infection of the membranes in the uterus and amniotic fluid. It presents with abdominal pain, uterine tenderness, vaginal discharge, fever, and maternal/foetal tachycardia.
Another key cause to remember is UTI.
It's managed with:
Sepsis 6 (Take – Lactate, Blood culture, Urine output. Give – O2, Abx, IVF)
Emergency c-section if signs of foetal distress
Cord Prolapse
Here, the umbilical cord descends below the presenting part of the foetus, therefore causing cord compression → foetal hypoxia.
Risk factors - Abnormal foetal lie, Multiple pregnancy, Polyhydramnios
It should always be suspected when there are signs of foetal distress on CTG. It is diagnosed on examination of the cervix. It's important to avoid trying to push the cord back as it can cause vasospasm!
Management:
Initially, it's important to try and relieve pressure on the cord:
Lie patient in left lateral position (with pillow under hip) or knee-chest position (on all fours) to draw foetus away from pelvis
Fill the bladder with fluid to push the foetal head away
If these don't work, other options include:
Emergency instrumental delivery or C-section
Tocolytics to stop uterine contractions
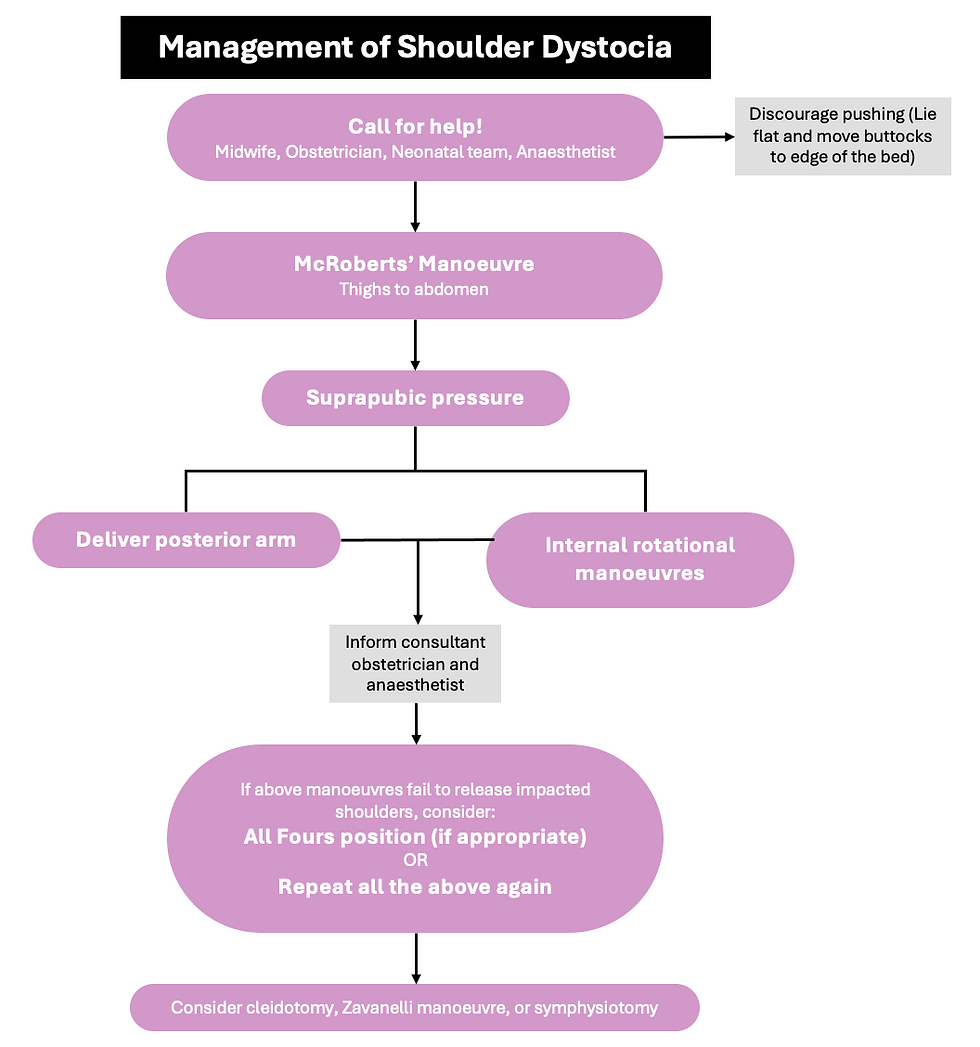
Shoulder Dystocia
This is where the anterior shoulder becomes stuck behind the pubic symphysis.
Risk factors - Macrosomia, GDM, Anticipation, Maternal birth weight, Maternal obesity
Anticipation - big baby, prolonged 1st/2nd stage, and instrumental delivery
It presents with:
Difficult delivery of the face and head
Failed descent of the shoulders following delivery of the head
Failure of restitution where the head remains face downwards and doesn’t turn back sideways as expected after delivery of it
Turtle-neck sign – Head is delivered but then retracts back into the vagina
The main complications that can occur here are:
Foetal hypoxia (and subsequent cerebral palsy)
Brachial plexus injury
Perineal tears
PPH
The 2 brachial plexus injuries that can occur here are:
Erb palsy (C5/C6) - more common
Klumpke palsy (C8/T1)
N.B. Erb’s palsy - C5 + C6 = 11 erbs and spices.