Reproductive System
Internal Reproductive Organs
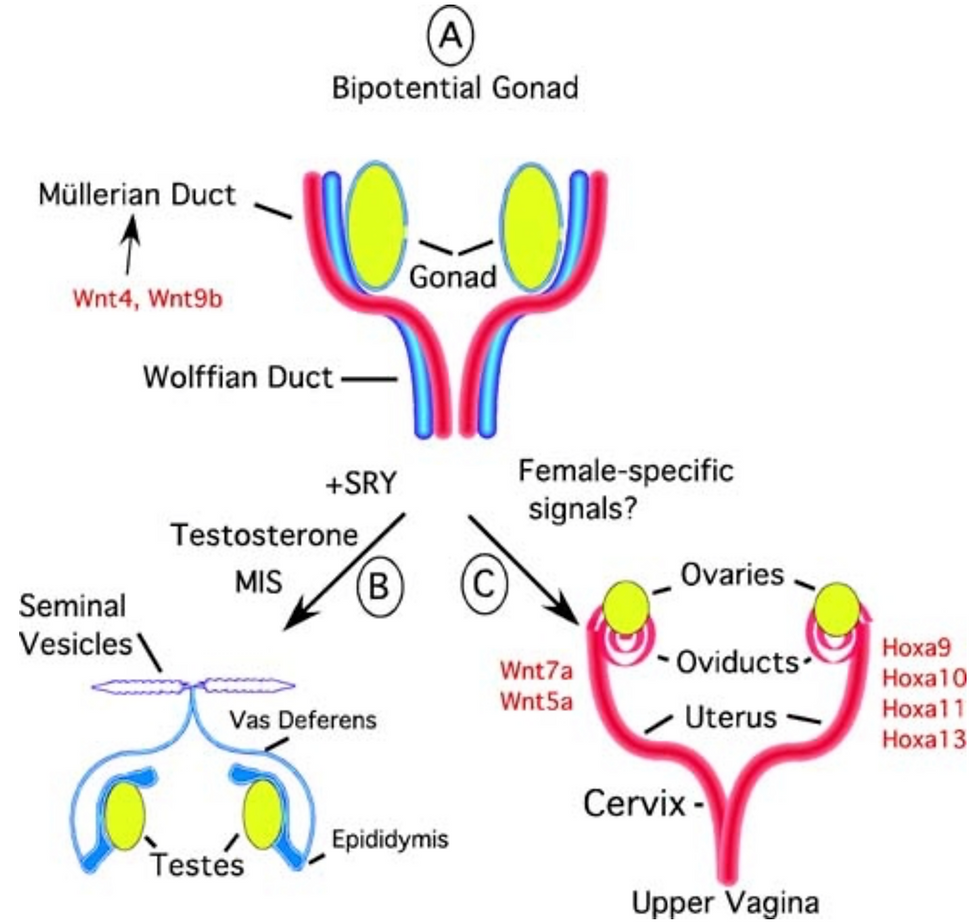
The female ducts are the Mullerian ducts, which go on to form the uterine tubes, uterus, and upper 1/3 vagina. It's inhibited in males by the presence of AMH (from Sertoli cells).
The male ducts are the Wolffian ducts, which go on to form the epididymis, vas deferens, seminal vesicles, and ejaculatory ducts. It's stimulated in males by the presence of Testosterone, but inhibited in females by the lack of testosterone (from Leydig cells).
External Reproductive Organs
For this to form, Testosterone is converted into DHT by 5-α-Reductase. This DHT binds to testosterone receptors with ↑efficacy (↑POTENCY), therefore leading to the differentiation into male external genitalia.
Gonadotrophins
Affect on the ovaries:
FSH causes Follicular maturation and growth
FSH receptors on Granulosa cells = Oestrogen synthesis
LH receptors on Theca cells = Androgen synthesis
When Oestrogen is high for a few days, there’s a temporary switch, causing LH surge → Ovulation
Corpus Luteum is rescued by hCG in pregnancy
Affect on the testes:
FSH receptors on Sertoli cells = Oestrogen synthesis
LH receptors on Leydig cells = Testosterone synthesis
Follicle
The Primordial Follicle is an oocyte surrounded by protective layers of Granulosa cells and a Basal Lamina.
Folliculogenesis is driven mostly by FSH, but early growth is independent of FSH (driven by local factors). Therefore, even with FSH suppression (e.g. with COCP), the follicles continue with early growth, but then die.
As the follicle grows, the Granulosa cells divide even more, forming gaps in the layers, which fill with follicular fluid to form an Antrum = Antral/Secondary Follicles.
Follicle Initiation and Recruitment - Cohort of early follicles leave the resting pool and grow continuously. They won’t continue to grow until they reach a sufficient size to respond to changes in FSH during the menstrual cycle
Only 1 follicle from the pool will be selected for Ovulation

Ovulation
This occurs because of the LH surge. Here, the basement membrane breaks so blood can pour into the middle, and the Oocyte-Cumulus complex breaks off and is caught by Fimbrae. Theca and Granulose cells then become mixed, forming the Corpus Luteum (CL).
Luteal Phase
This phases mainly produces Progesterone, which works to:
Ready the endometrium for implantation
Thicken the cervical mucous to prevent further sperm penetration
Suppress cilia in the Uterine tubes once the Oocyte has passed
Oestrogen is also produced here to maintain the endometrium.
The CL has a finite lifespan of 14 days if no fertilisation occurs. With this, there's a subsequent regression and fall in progesterone, which is necessary to initiate new cycle (Inter-cycle rise in FSH). The CL is rescued in pregnancy by hCG, which binds to LH receptors for more Progesterone production.
If the CL isn't continued, there's apoptosis, vasculature breakdown, leading to the CL shrinking to become the Corpus Albicans.